TMJ PAIN, FIBROMYALGIA AND CHRONIC FATIGUE SYNDROME
by Dr John Utama - Dentist, BDS MBA
 Chronic pain is the bane of millions of people’s existence, it’s classified as a disease sharing similar signs and symptoms with other chronic conditions such as fibromyalgia (FM), irritable bowel syndrome, osteoarthritis, interstitial cystitis and chronic fatigue syndrome.
Chronic pain is the bane of millions of people’s existence, it’s classified as a disease sharing similar signs and symptoms with other chronic conditions such as fibromyalgia (FM), irritable bowel syndrome, osteoarthritis, interstitial cystitis and chronic fatigue syndrome.
Chronic pain sufferers describe their daily dose of aches all over the body, experiencing pain in the muscles and joints in particular around the face, neck, shoulder, back and hip areas. Many complain of restlessness at night associated with little quality of sleep, others experience mood disturbances and episodes of depression.
The Dental Connection
 Several studies (1,2,3) show in particular, the coexistence between fibromyalgia and TMJ Dysfunction (TMD), hence the dental connection.
Several studies (1,2,3) show in particular, the coexistence between fibromyalgia and TMJ Dysfunction (TMD), hence the dental connection.
Before we go any further, it’s important to distinguish between peripheral (acute) pain and central sensitisation (chronic pain).
Peripheral Pain
If you inadvertently touch a hot stove with your hand, you will instantly pull your hand away to avoid injury. If you weren’t fast enough, you will burn your hand and it will be painful to touch for a few days. This condition is called allodynia, whereby a gentle touch to an injured part of the body stimulates a painful reaction, which it normally doesn’t cause pain when the body is uninjured. Similarly, any painful stimuli will be exaggerated (hyperalgesia). This is a protective function of pain, to allow the body to heal after an injury. With the absence of any further damage to the tissue, the body will go back to normal soon after. Peripheral pain is almost exclusively localised at the origin of the tissue damage.
Central Sensitisation
Chronic pain occurs when there is a continuous bombardment of pain stimuli onto the same part of the body. If stimulated long enough (long-term potentiation), the central nervous system (CNS: brain and spinal cord) will undergo irreversible changes, this is called central sensitisation. The intensity, duration and frequency of the pain stimuli determine the severity of the chronic pain, and the pain tends to be more generalised; the site of the pain is at a distance from the origin of the pain stimuli and multiple painful sites may be present. Now we begin to see the signs and symptoms of chronic pain described above, where the body aches all over. This renders chronic pain most difficult to diagnose, as in the case of FM.
As cited in the studies above, TMD shares many of the signs and symptoms of FM, with the foci in the head and neck regions. Having treated many TMD cases, I find the conclusions of the aforementioned studies are consistent with the medical histories of my own patients, i.e., most of my TMD patients have either FM or chronic fatigue syndrome.
Here are some other signs and symptoms shared by chronic pain sufferers:
- Head-aches/migraines
- Dryness in mouth, nose, and eyes
- Hypersensitivity to cold and/or heat
- Difficulty in focus (“brain fog")
- Incontinence
- Numbness or tingling in the fingers and feet
- Joint stiffness
- Stomach upsets
Connecting The Dots
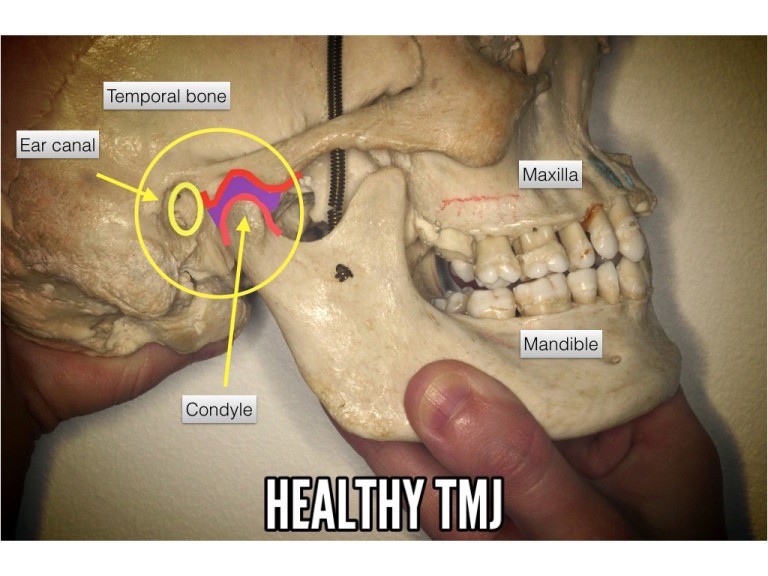
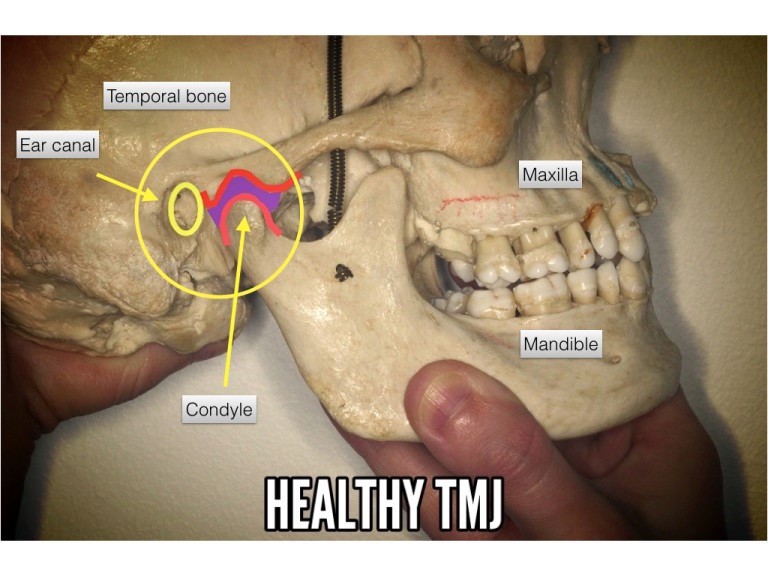
As hypothesized above, chronic pain develops when there are continuous, unrelenting pain stimuli attacking the body, effecting changes in the CNS. It is feasible that malocclusion (noxious bite) may contribute to the central sensitisation. The diagram below shows a healthy TMJ with space (illustrated in purple) between the condyle and the base of the temporal bone. The TMJ space accommodates nerves, blood vessels, ligaments and muscles.
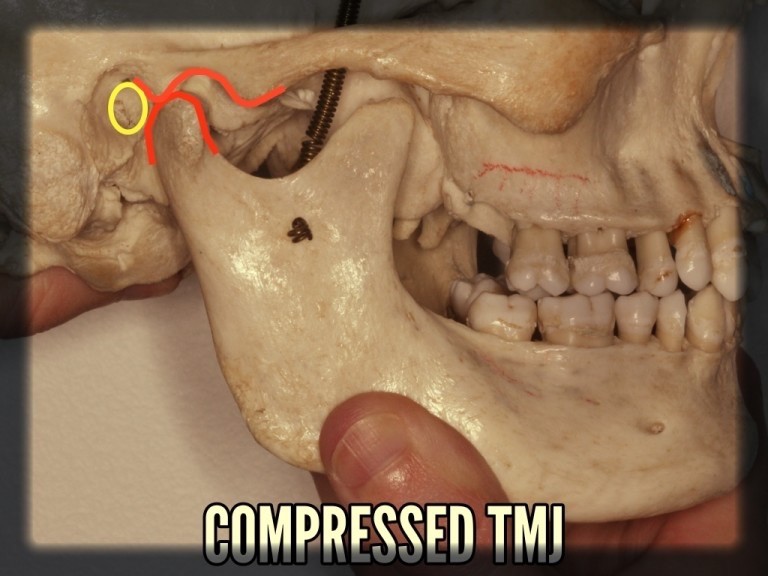
The TMJ space below is compressed, usually in the presence of a noxious bite. This occurs when the lower jaw (mandible) is forced back during the daily chewing and swallowing activities. These activities may occur two to three thousand times a day; furthermore, many TMD and FM patients tend to clench their teeth while asleep. It is feasible that these activities represent the trigger to chronic pain, compressing the nerves and other vital structures multiple times throughout the course of the day (and night).
Management Of TMD
Sir William Osler said:
"What you don’t know, you don’t diagnose"
Phase 1
Splint therapy
Night and day splints
The most important phase in the management of TMD is to decompress the TMJs and to create space between the condyle and the temporal bone. Depending on the severity of the condition, both day and night splints may be required. The patient must wear the day splint all day including eating (most important time to wear the splint). The night splint is to be worn at night time to stop clenching.
Phase 2
Weaning off the splints may be possible, but ultimately it depends on the severity of the malocclusion in the first place.
Other options are fixed crowns/bridges/implants or orthodontic treatment. Both options are designed to correct the bite, creating the optimal TMJ spaces.
Based on the coexistence of TMD and FM, it is feasible to expect that treatment of TMD would have significant benefits on FM. More studies are required to support this hypothesis.
Conclusion
Several studies have found a link between TMJ pain and fibromyalgia (FM). Both share similar signs and symptoms with chronic pain or central sensitisation being the most common in both conditions. Treatment of TMJs may alleviate some of the debilitating pain sustained by FM sufferers.
References
- Signs and symptoms of temporomandibular dysfunction in fibromyalgic patients.Fraga BP1, Santos EB, Farias Neto JP, Macieira JC, Quintans LJ Jr, Onofre AS, De Santana JM, Martins-Filho PR, Bonjardim LR. J Craniofac Surg. 2012 Mar;23(2):615-8. doi: 10.1097/SCS.0b013e31824cd81a.
- Coexistence of fibromyalgia, temporomandibular disorder, and masticatory myofascial pain syndromes.
Leblebici B1, Pektaş ZO, Ortancil O, Hürcan EC, Bagis S, Akman MN. Rheumatol Int. 2007 Apr;27(6):541-4. Epub 2006 Nov 10. - Comparison of masticatory dysfunction in temporomandibular disorders and fibromyalgia.
[Article in English, Italian]
Manfredini D1, Tognini F, Montagnani G, Bazzichi L, Bombardieri S, Bosco M.
Minerva Stomatol. 2004 Nov-Dec;53(11-12):641-50.